
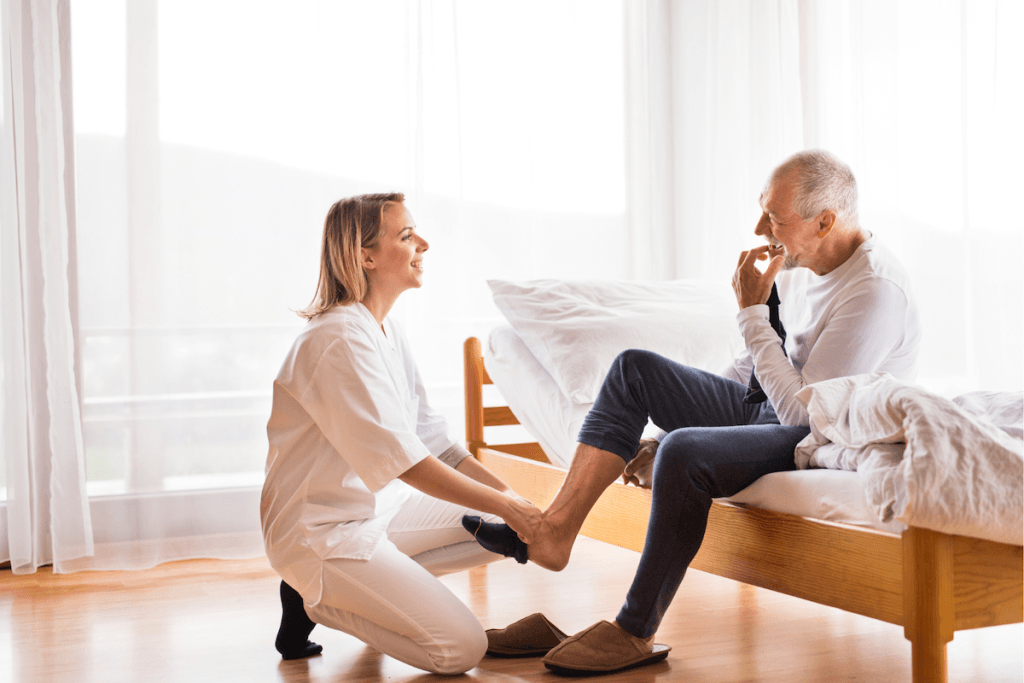
Diabetes & feet
Essential foot care for Diabetes
Diabetes–related foot complications can have a significant impact on both physical health and overall well-being.
Nerve damage (neuropathy) can cause numbness, reducing the ability to feel pain or temperature changes, which increases the risk of unnoticed injuries.
Poor circulation further slows healing, making even minor cuts or blisters prone to infection, potentially leading to ulcers and, in severe cases, amputation.
Beyond the physical effects, these complications can take an emotional and psychological toll. Chronic foot pain, limited mobility and the fear of serious infections can lead to anxiety, depression and reduced independence.
Everyday activities such as walking, exercising or even wearing shoes comfortably may become challenging, affecting overall quality of life.
Early detection and proper foot care play a crucial role in preventing these complications.
Regular check-ups with a podiatrist, maintaining good blood sugar control and practicing daily foot hygiene can help protect both physical health and personal well-being, allowing individuals to stay active and maintain their independence.
Our experienced podiatrists specialise in diabetic foot assessments, wound care and prevention strategies.
We provide expert advice on proper footwear, nail care and daily foot checks to help you stay active and pain-free.
If you have diabetes, regular foot check-ups are crucial. Book an appointment today to safeguard your foot health.
Diabetes foot assessments include
01
Testing blood flow and circulation
02
Testing nerve sensation
03
Identifying skin or nail problems
Diabetes & foot health FAQs
Diabetes can cause nerve damage (neuropathy) and reduced circulation, making it harder to feel injuries and slowing down the healing process. Without proper care, even small cuts or blisters can develop into serious infections.
High blood sugar levels over time can damage the nerves in your feet, leading to numbness, tingling, burning sensations or loss of feeling. This condition, known as diabetic neuropathy, increases the risk of unnoticed injuries.
Symptoms of reduced blood flow include cold feet, slow-healing wounds, dry skin, cramping and changes in skin color. Poor circulation can make it harder for injuries to heal and increases the risk of ulcers and infections.
It’s important to check your feet daily for cuts, blisters, redness, swelling or sores. If you notice any wounds that aren’t healing or signs of infection, seek medical attention immediately.
Diabetic-friendly shoes should be well-fitted, supportive, have a wide toe box and minimal seams to prevent pressure points and friction. Avoid tight, narrow shoes and always wear socks to protect your feet.
Yes, but it’s best to follow the contour of your toes and avoid cutting too short to prevent ingrown toenails. If you have trouble trimming your nails or have thickened nails, a podiatrist can help.
Regular podiatry check-ups (at least once a year) are recommended for people with diabetes. If you have neuropathy, circulation issues or a history of foot ulcers, more frequent visits are necessary.
Yes. If left untreated, diabetic foot complications can lead to infections, ulcers and in severe cases, amputation. Early detection and proper care can prevent these serious outcomes.
Recent evidence based Australian Guidelines have a strong recommendation for regular podiatry assessment for people with diabetes. More information can be found here


